A lot has been written about Glycemic Index. This has been done to ensure that the mainstream keeps pushing the nonsensical HIGH CARB LOW FAT (HCLF) diet to everyone, under the garb of being “Healthy and Balanced” – diabetics are no exception.
Diabetes is a problem of ‘inability to process carbs’. Yet, the high priests of the food and drug industry keep pushing the HCLF diet to make sure that personal profits at the expense of public health are secured; GI forms the base of their incorrect arguments.
Dr Bernstein categorically said in one of his videos, that a lot of nonsense is going on in nutrition circles regarding the Glycemic Index. Let’s see why.
Glycemic Index and Glycemic Load
When it comes to looking at insulin needs, it makes more sense to focus on GL rather than GI. But, even GL is not enough on its own. For example, in 100 gram of each (data from fatsecret.com):
GL of Apple = GI*Carbs/100 = 38*11.41/100 = 4.34.
GL of Watermelon = GI*Carbs/100 = 72*7.15/100 = 5.15.
So, the need for insulin will be determined by net carbs, and not GI or GL. GI for the same GL will only control the Post Prandial Glucose Excursion (PPGE) and not the total insulin need. Also, it will govern the type of insulin used –ultra fast acting versus rapid acting — for controlling PPGE. This has been highlighted in the following study on Type 1
CONCLUSIONS—Low–glycemic index meals produce a lower PPGE than high–glycemic index meals. Preprandial ultra-short-acting insulin is the optimal therapy for a low–glycemic index meal.
I always look at insulin needs from the perspective of Type 1 diabetics as they have to rely on exogenous insulin. Does a low GI diet reduce overall insulin needs? Logically it cannot, because to process the same amount of carbs (or insulinogenic component — more about this later) one will need the same amount of insulin. The only thing that is dependent on GI is the PPGE versus the type of insulin used. In addition, the AUC will be controlled by GI/GL combination and the type of insulin used.
According to GI and GL theory, one can eat a lot of low GI (carb) food for a moderate GL. Sure, the PPGE values would be better, but does it reduce the need of insulin? No. For example, Pasta has a GL of 20 (as minimum, though it can vary) but does that mean eating the same amount of carbs and proteins from some other source (with total GL being higher) will increase the insulin requirement? Does it solve the problem of higher insulin needs irrespective of GI/GL? NOPE. Not happening!
Unfortunately, since mainstream never focuses on insulin, they keep peddling this GI and GL nonsense over and over again. I’m not sure why these so called experts find it so difficult to wrap their heads around this. It is not rocket science.
In addition, despite the failure of the 13 year LookAHEAD Protocol study, they keep promoting the ‘eat less move more’ myth. Now these so called researchers are suggesting another insanity — office desk should be equipped with pedals. All this makes it so evident that all those pushing the horrible HCLF diet to diabetics won’t let it go as they are religiously married to industry dollars.
This harping on GI doesn’t even help with obesity as is evident from the following study:
An 18-mo randomized trial of a low-glycemic-index diet and weight change in Brazilian women.
CONCLUSIONS: Long-term weight changes were not significantly different between the HGI and LGI diet groups; therefore, this study does not support a benefit of an LGI diet for weight control. Favorable changes in lipids confirmed previous results.
So, let’s bury all the myth around GI once and forever. As far as diabetes, obesity, insulin resistance, PCOS etc are concerned, it’s all about managing the residual insulin levels in blood and all the experts are barking up the wrong tree. Intentionally. I say intentionally because the day insulin comes into focus, their so called healthy and balanced diet will turn out to be the most horrible diet on the planet.
But What About Insulin Load?
There are too many factors which complicate the issue of insulin needs when it comes to an actual meal. This is because proteins and fats, in non-negligible quantities, are always a part of the usual meal. Both of them reduce the GL value. However, protein complicates the issue as it is also insulinogenic — ie it triggers an insulin response. Not all animal proteins behave similarly. Some have a high insulinogenic component whereas some have lower.
A high insulinogenic meal would mean that one would need higher insulin levels to process the meal. Sustained high levels of insulin is a stepping stone to insulin resistance, obesity and metabolic syndrome problems.
54% of all the proteins are converted into glucose. This is why Type 1 diabetics have to account for proteins in their diet along with carbs. So from an “insulinogenic load” point of view we are looking at:
Insulin load of meal = carbs – fiber + 0.54*proteins.
This should clearly help in understanding how much insulin response triggering food we are ingesting. The regular HCLF meal with 60% carbs, 20% proteins and 20% fat would mean
Insulinogenic load HCLF Meal = 60% - 5% (fiber) + 0.54*20 = 55% + 10.8% = 65.8%
How does LCHF Help?
The LCHF that we talk on dLife.in is based on the premise of 20% carbs, 20% Proteins and 60% Fats, respectively. Presuming around 15 g fiber intake from such a meal,
Insulinogenic load of LCHF meal = 20% - 3% + 0.54*20 = 27.8%
Right away we see a 38% reduction in the insulinogenic load of the meals. From the ketogenic diet (subset of LCHF) perspective, which considers that 10% of fat is also anti-ketogenic, we can compute the difference between HCLF and LCHF insulinogenic load to be 34%. This is precisely why managing blood sugar becomes easier on an LCHF diet. This is just an alternative way of looking at this article. Any which way one looks at it, the LCHF diet comes out on top.
When I first came up with 20:20:60 it was based on a Swedish study which concluded that at 20% max Carbohydrate, SFA has no relation with CVD. Then, from 2013 onwards, after being on it for 18 months, I started talking about it on forums. There’s an interesting comment from an engineer who is also a low carb proponent; he based his conclusion on the following chart on his site:
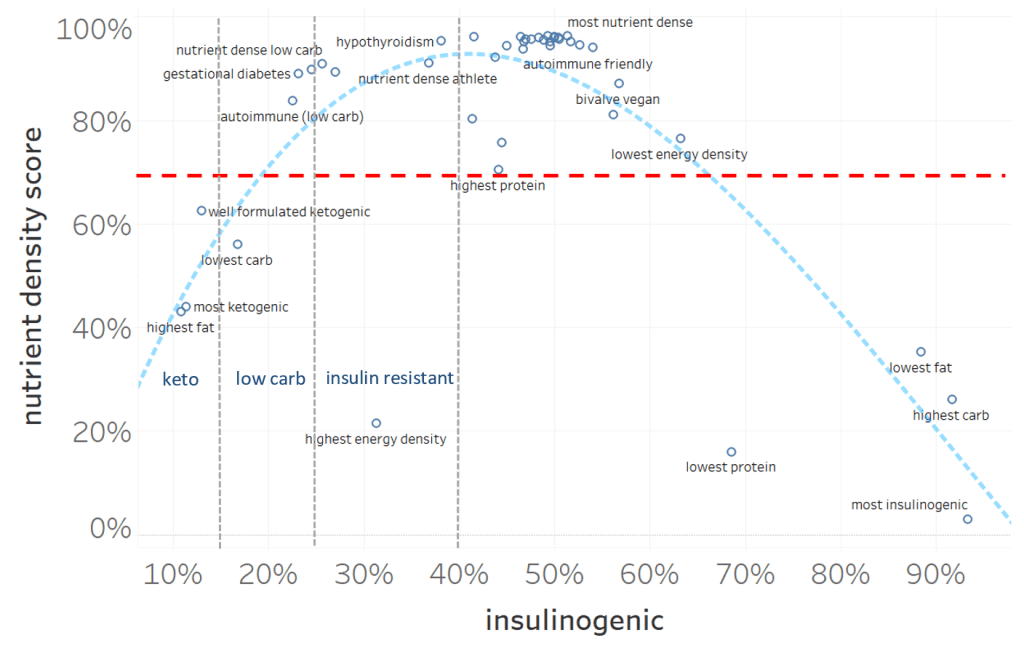
All those who are struggling with insulin resistance should aim for a 40% max insulinogenic component in the meal. We never knew this back then, but in hindsight we find we are far below that number. As a result, it is not surprising that we have clocked 200+ success stories of type 2 diabetes reversal, 3 cases of well managed type 1 diabetics and weight loss success stories ranging from 5 kg to 35 kg.
Based on the graph above, the LCHF diet is supposed to restrict the insulinogenic response at 25% max. However, our standard of 20:20:60 (leading to around 28%) has worked well and has an exceptional compliance rate – possibly because the Indian diet is not beef-and-bacon centric, which means that hitting even 20% protein is difficult for many.
Special mention is needed for Type 1 diabetics who always have to rely on exogenous insulin. The HCLF diet peddled by nutritionists and dietitians is the worst possible diet for a diabetic. The diet converts the whole body of a type 1 diabetic into a glucose sump instead of letting the liver do the job.
When industrial doses of insulin are used to cover high carbs, this leads to peripheral hyperinsulinemia, and that has its own damaging effect. But in order to sell HCLF, the high priests of the food and drug industry go with a systemic increase in insulin by injecting subcutaneously in type 1 or through pancreas whipping drugs and/or insulin in type 2.
However, Shalini and Srishti‘s insulin consumption came down drastically on low-carb and yet they land A1Cs of 5.4/5.7. Most importantly, they are aiming for lower swings around the eABG (computed from A1C) which is also important to keep diabetic complications to minimal levels. This is only possible on a low-carb diet in line with Dr Bernstein’s law of small numbers, and not the HCLF crap.
Wrapping Up
- HCLF diet is the worst for controlling blood sugars.
- LCHF diet helps in normalizing blood sugars with least dependence on drugs.
- Insulin resistance and peripheral hyperinsulinemia are reduced on LCHF diet.
- GI is a useless science. So is GL. Neither of them help in reducing insulin needs.
- Keep insulinogenic component of diet under 30%. Our 20:20:60 thumb rule fits well as exemplified by a huge number of success stories.
- Focus on fasting insulin and PP insulin levels.
Reference
- https://ses.library.usyd.edu.au/handle/2123/11945
- https://www.dlife.in/forums/threads/beyond-glycemic-index-the-new-food-insulin-index.19/
- http://high-fat-nutrition.blogspot.com/2014/12/accord-and-musings-on-insulin.html